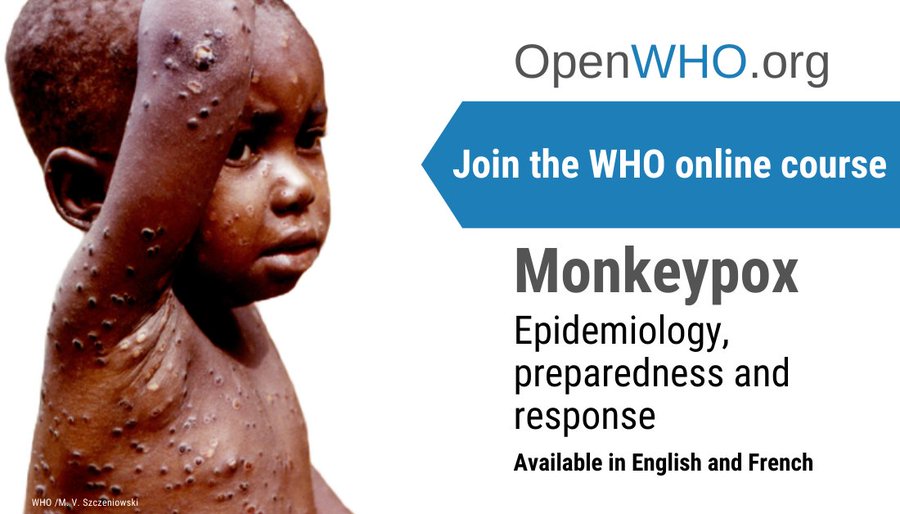
European outbreak of monkeypox: what you need to know
Four new cases of monkeypox have been reported in the UK, bringing the total number of confirmed cases to seven. The UK Health Security Agency (UKHSA) is urgently looking for the source of the outbreak
Estimated reading time: 8 minutes
Michael Head, University of Southampton
The first case in the current outbreak was confirmed on May 6. But this is not the first time monkeypox has been reported in the UK. Three cases were also reported in 2021 and one in 2018. However, these infections are rarely seen in the UK and are overwhelmingly linked to international travel from endemic areas, including parts of west and central Africa.
On May 18 five cases of monkeypox were reported in Portugal, with investigations into 20 further suspected cases. On the same day, the Spanish health authorities reported eight suspected cases in men who have sex with men.
This is the largest monkeypox outbreak ever seen in Europe. It is not known if the cases are linked.
Misnomer
Monkeypox, as the name suggests, was first found in laboratory monkeys in the late 1950s. However, scientists aren’t sure if monkeys are the main animal reservoirs (carriers of the virus), so the name may be a bit of a misnomer. The latest thinking is that the main reservoir is probably smaller animals, such as rodents.

Unlike COVID, monkeypox does not spread easily from human to human. It typically requires interaction with animals that carry the virus, or being in very close contact with infected people, or having contact with “fomites” (such as contaminated clothes, towels or furniture). Also unlike COVID, monkeypox is not known to spread asymptomatically. However, the evidence on monkeypox is thin, and the current outbreaks will provide new knowledge around its impact and transmission.
Monkeypox belongs to the same family of viruses as smallpox, but is less transmissible. People who catch it typically develop a fever and a distinctive rash and blisters. The disease is usually self-limiting, with symptoms disappearing after a few weeks. However, monkeypox can cause severe illness, with outbreaks typically showing a case-fatality rate (the proportion of people with the disease who die from it) of between 1% and 15%, with severe disease and death more likely among children.
Sexually transmitted?
The UKHSA says that some cases in the May 2022 outbreak cannot be explained by recent international travel, suggesting that there has probably been some “community transmission”. Four of the seven cases are in people who identify as gay, bisexual or other men who have sex with men. A UKHSA epidemiologist tweeted that this is “highly suggestive of spread in sexual networks”. The cases in Spain may also fall under similar consideration.
So the transmission here may be a little unusual compared with previous outbreaks. While there is a lot we don’t know about monkeypox, we do know the virus can be transmitted via close contact, for example, including prolonged skin-to-skin contact.
There is no evidence that it is a sexually transmitted infection in the manner of HIV or chlamydia. It’s more that, in the UK outbreak, the close contact during sexual or intimate activity may have been a key factor during transmission.
This may be the first time transmission of monkeypox via sexual contact or intimate activity has been documented. But the implications are not so significant in that we know close contact is required for transmission. The social dynamics around the transmission of infectious diseases means this finding may be most useful for the public health teams involved in “contact tracing” – finding other people who may have been exposed to the virus.
Very low risks for the general public
The monkeypox risks to the wider UK public are extremely low, and the NHS has specialist units that focus on treating these sorts of tropical infections. And, thankfully, there are ways of bringing the virus to heel.
The US Centers for Disease Control and Prevention highlights how the smallpox vaccine, cidofovir (an anti-viral drug), and vaccinia immune globulin can be used to control a monkeypox outbreak.
However, beyond the smallpox vaccine, there is no specific vaccine to protect against monkeypox. Some experts have suggested that stopping widespread vaccination against smallpox might have lowered population immunity against monkeypox, thus making cases and outbreaks more likely.
A 2019 meeting at Chatham House in London suggested that an unintended consequence of smallpox eradication could be that “emergent or re-emergent human monkeypox might fill the epidemiological niche vacated by smallpox”.
However, these imported monkeypox cases and other tropical infections (such as Ebola, malaria and Lassa fever) indicate a wider burden of disease elsewhere in the world, typically in low-income countries with limited access to healthcare. It may be that in a post-pandemic environment, we should give more consideration to understanding the local and global implications of Lassa, monkeypox, Ebola and other rare but serious pathogens.
Michael Head, Senior Research Fellow in Global Health, University of Southampton
This article is republished from The Conversation under a Creative Commons license. Read the original article.
What's Your Reaction?